This fact sheet explains a method of introducing eggs and sperm, called ICSI, that is commonly used in IVF when the characteristics of the sperm sample are outside of normal ranges.
What is ICSI?
ICSI is a method of insemination commonly used in IVF when the characteristics of the sperm sample are outside of normal ranges. It is very similar to conventional IVF insemination except instead of mixing the eggs and sperm together in a dish so the sperm fertilises the egg ‘naturally’, a single sperm is injected directly into each egg. The first pregnancies following ICSI were reported in 1991 and the first baby was born in 1992. Since then ICSI has become widely used in fertility clinics worldwide.
Why do we need ICSI?
In conventional IVF insemination, we need very large numbers of actively swimming normal sperm to have a chance that eggs will fertilise. For many couples, the number of suitable sperm that are available may be very limited or there may be other factors preventing fertilisation. ICSI gives hope in these cases as very few sperm are needed and the sperm’s ability to penetrate the egg itself is no longer important.
We may recommend ICSI if:
- The man’s sperm count is very low
- The sperm have poor motility (movement) or are in other ways abnormal
- The sperm has been retrieved surgically from the epididymis (PESA) or the testes (TESA) or needs to be extracted from urine after retrograde or electro-ejaculation
- There are high levels of antisperm antibodies in the semen
- If your previous IVF treatment using standard IVF insemination failed to achieve fertilisation.
How is ICSI performed?
After the man’s semen sample has been provided to the lab, our scientists separate the sperm from the ejaculate. Commonly this is a fresh semen sample, but in some cases, we use pre-frozen and thawed sperm.
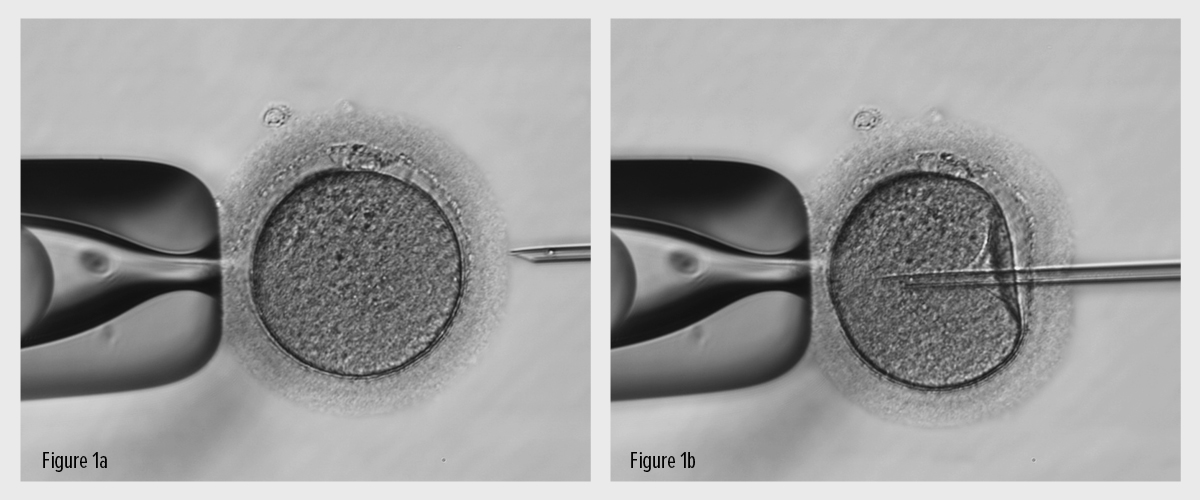
Not long after the woman’s eggs have been collected, using a high magnification microscope and specialist microinjection equipment, the scientist selects a single sperm and injects it directly into each mature egg with a fine glass needle. (Fig.1).
Figure 1: The egg is held by a glass pipette (left hand side) and a single sperm (in the tip of needle on right hand side) is injected through the shell and into the egg.
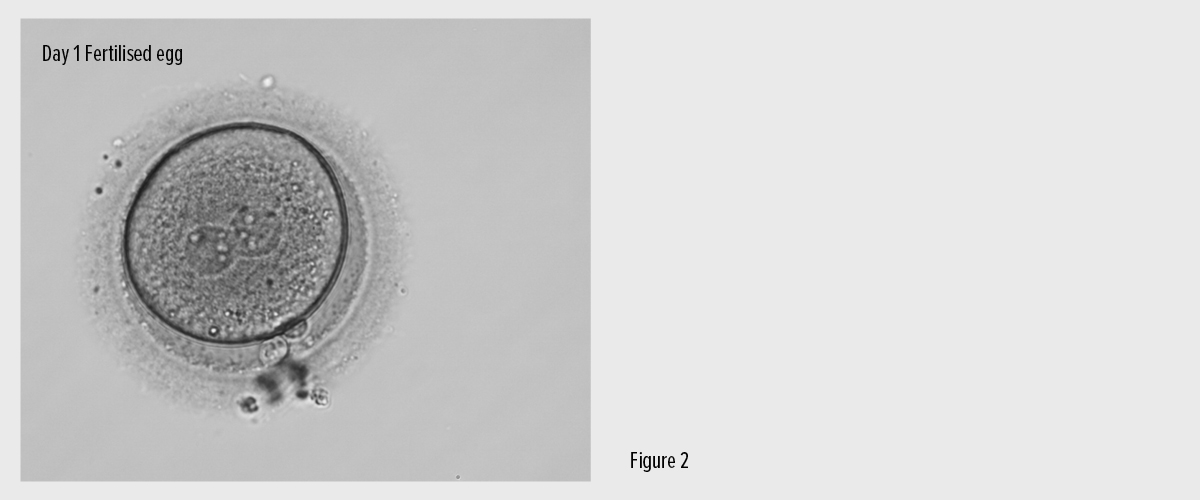
The following day those eggs that have fertilised normally are identified and cultured in the laboratory (Fig. 2).
Figure 2: A fertilised egg the day after egg collection and ICSI.
Does ICSI change any other aspects of IVF treatment?
No. All other phases of the treatment cycle are the same. You can read more in our IVF step-by-step fact sheet.
How successful is ICSI?
ICSI does not guarantee that eggs will be fertilised as the normal cell processes still need to happen once the sperm has been placed in the egg. ICSI does however greatly increase the chances for patients who would not have achieved fertilisation by other means.
About 70% of eggs are successfully fertilised using ICSI and more than 95% of patients who have ICSI will achieve fertilisation in at least some eggs. In most of these cases, fertilisation would not have been possible without ICSI.
The resulting likelihood of achieving a successful pregnancy using ICSI varies between patients, particularly depending on the age of the woman but, worldwide, about 25% of patients will have a baby after one attempt at ICSI.
Are babies born through ICSI at any greater risks?
This is naturally a concern for you and there has been some confusing media attention. The consensus from recent medical literature suggests that the risks are the same as for conventional IVF.
You should be aware though that there are potentially some risks caused by the underlying male infertility problems rather than from the ICSI process itself. These include:
Congenital bilateral absence of the vas deferens (CBAVD)
Some men are infertile because they do not have vas deferens. These are the ducts that transport sperm from the testicles to the base of the penis. Without these, the sperm, which are created in the testicles, cannot get out and total infertility results. Men with CBAVD have been found to be more likely to carry the cystic fibrosis gene and there is a risk that this may be passed on to any children if you use ICSI.
If we suspect you have this congenital condition, we will discuss your risks in more detail and we may recommend testing. As the cystic fibrosis gene is quite common in the general Caucasian population (about 1 in 25 people are carriers), we may also test your partner to assess the risk of passing on cystic fibrosis to
any children.
Deletions on the Y chromosome
Occasionally men with a very low sperm count (less than 1 million sperm per ml) may have an abnormality in the Y chromosome. This means that any son born (whether the child is born by IVF or ICSI or natural conception) may have the same sub-fertility problem as his father. If your sperm count is low, we can check if this is the case with genetic testing.
Other chromosomal abnormalities
There seems to be a very small increase in the risk of chromosome abnormalities among children born following ICSI. The overall incidence following ICSI treatment is reported to be 1.6% compared to 0.8% in the general population.
This is thought to be a result of abnormalities that have caused the man’s infertility, rather than from the ICSI procedure itself. This especially applies to sex chromosome abnormalities, which are more common when the semen analysis is severely abnormal.
Contact Life Fertility Clinic
The friendly and professional team at Life Fertility Clinic are happy to answer any other questions you have about this treatment. Although there are very small risks in using sperm that might not otherwise naturally fertilise an egg, it has proved to be a successful way for many couples to have a healthy child that is biologically related to both of them.
