If your fertility specialist has recommended that that your embryos are cultured to the ‘blastocyst stage’ as part of your IVF treatment, this fact sheet will explain what that means and how it may improve the chances of a successful outcome.
What is a blastocyst?
The word ‘blastocyst’ refers to the stage that the human embryo reaches approximately five to six days after fertilisation (Fig.1).
Figure 1: A blastocyst stage embryo.
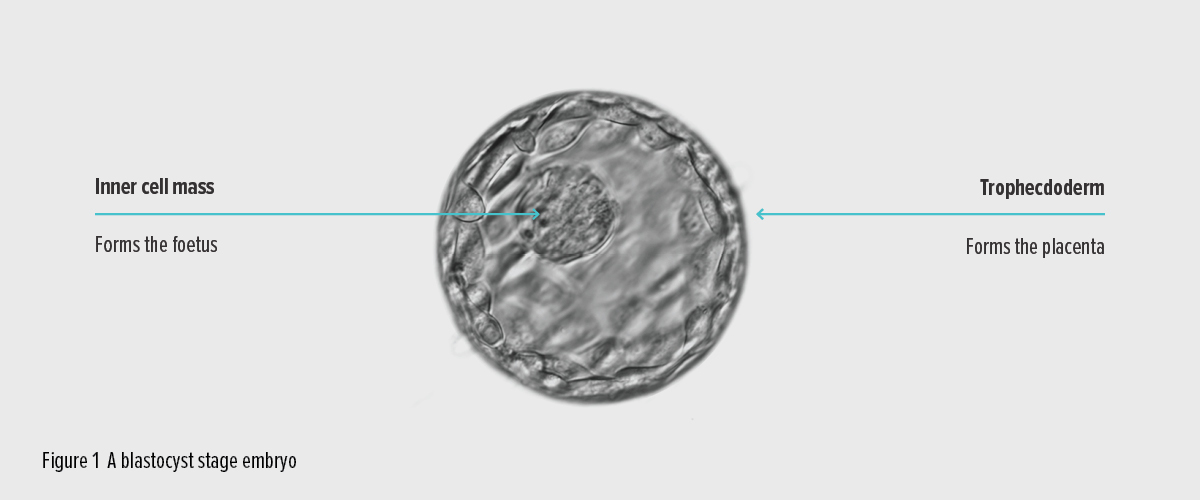
The embryo must reach this stage before it can hatch and implant in the lining of the uterus. The blastocyst stage embryo typically has between 50 and 200 cells. Some of these cells (the trophectoderm) have a role in implanting into the uterus and some (the inner cell mass) are the early cells of the foetus itself.
In a natural pregnancy, the fertilised egg develops into a blastocyst as it travels along the fallopian tube towards the uterus (Fig. 2).
Figure 2: From egg to blastocyst in the female reproductive tract.
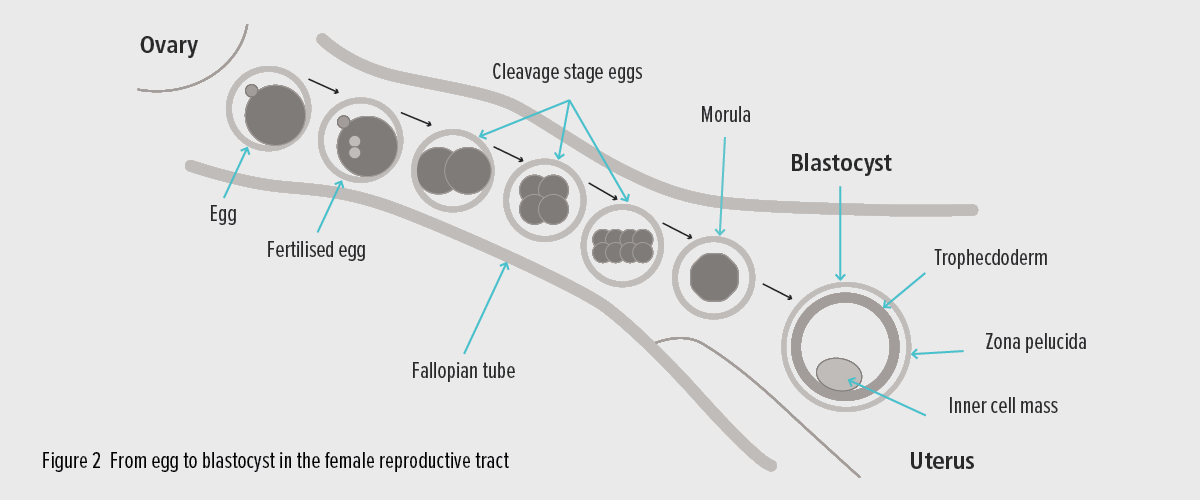
The egg is fertilised after it is released from the ovary and the embryo divides as it travels along the fallopian tube. It reaches blastocyst stage as it enters the uterus.
What is blastocyst culture?
Until about 10 years ago it was not possible to consistently grow (or ‘culture’) embryos to the blastocyst stage in a laboratory. Specialised commercial culture media (the fluid in which embryos are grown in the lab) have now made it possible to successfully nurture embryos to the blastocyst stage outside the human body. This laboratory process is known as ‘blastocyst culture’.
How does blastocyst culture improve IVF outcomes?
Standard practice in IVF used to be to replace embryos into the uterus after only two or three days of development, when the embryos are at the ‘cleavage stages’ and usually composed of somewhere between two and eight cells.
Extending the embryo culture to five or six days gives the scientists a longer period over which to observe embryo development. During this extra couple of days it is completely normal for only some embryos to progress and develop to form a blastocyst. Blastocysts are therefore a more select bunch, so have a greater potential to form a pregnancy than embryos at earlier cleavage stages.
It is also thought that transferring an embryo into the uterus at the blastocyst stage may improve its chance of implanting because we are getting the timing right. The blastocyst is the stage of development that would normally be in the uterus ready to implant. Cleavage stage embryos on the other hand would normally be in the fallopian tube, so when we put them back into the uterus they have to hang around for a couple of days before they can implant.
In the early days of IVF, doctors often transferred a number of embryos into the uterus to allow for the ones that wouldn’t develop successfully and this resulted in multiple births for some women. Most importantly, with blastocyst culture, as we are being more selective in our choice of embryo, we can confidently transfer fewer, often single embryos and avoid multiple pregnancies.
How many embryos reach the blastocyst stage?
The proportion of embryos that successfully develop to blastocyst stage varies a lot between patients. We know that many embryos never develop beyond the early stages but it is often impossible to tell which ones that will be by looking at them.
A typical example might be that we retrieve 10 eggs from a woman and manage to successfully fertilise eight in the laboratory. By the third day, six of the embryos may appear to be developing normally and it is impossible to choose which might be the best option to implant. By day five, only three of those embryos will have successfully formed a normal blastocyst.
Does everyone get blastocysts to transfer?
More often than not there is at least one healthy blastocyst after the culture period, however it is possible for none of a group of embryos to make it to the blastocyst stage.
As far as we can tell, those embryos that fail to thrive and reach the blastocyst stage in the laboratory are most likely to have also failed in the uterus had they been replaced at an earlier stage. So, while not having blastocysts to transfer can be extremely disappointing, on reflection most people would prefer to know at this stage rather than go through the expense, uncertainty and medications of the embryo transfer process only to find the pregnancy test is negative.
Similarly, if you are hoping to preserve some extra embryos for a future pregnancy, you may find the number of ‘spare’ blastocysts is limited, however, any that have progressed and can be frozen will give you the best chance of pregnancy in future.
Is blastocyst culture right for me?
We currently recommend blastocyst transfer to most patients who have a good chance of developing one or more healthy blastocysts.
If we have managed to retrieve fewer than normal eggs or fewer than normal have fertilised or are developing normally
by the third day, we will discuss the situation with you and you may choose to have an embryo implanted at an earlier stage.
If you are planning a frozen embryo transfer cycle using embryos frozen in previous cycles at an earlier stage of development, we can use blastocyst culture to see which of those thawed embryos progresses to the blastocyst stage and has the best chance of pregnancy before transferring the embryo(s).
Contact Life Fertility Clinic
The friendly and professional team at Life Fertility Clinic are happy to answer any other questions you may have about whether blastocyst culture and transfer is the best option for you.
